Miscarriage: making the diagnosis
The physical and psychological effects of miscarriage for a woman and her family are often under appreciated. The journey from unexpected bleeding to diagnosis, deciding the right treatment for you, and then the medical and emotional aftercare, is a difficult one.
Sadly, miscarriage happens in around 15% or 1-in-6 pregnancies that have been ‘clinically recognised’. This means a positive pregnancy test, a missed period and possibly symptoms of early pregnancy. The true rate is even higher for very early losses - ones that might not be recognised by the person trying for pregnancy. These include what is sometimes called ‘biochemical pregnancies’ - when there’s a weakly positive test that then goes negative, with minimal extra bleeding than a period.
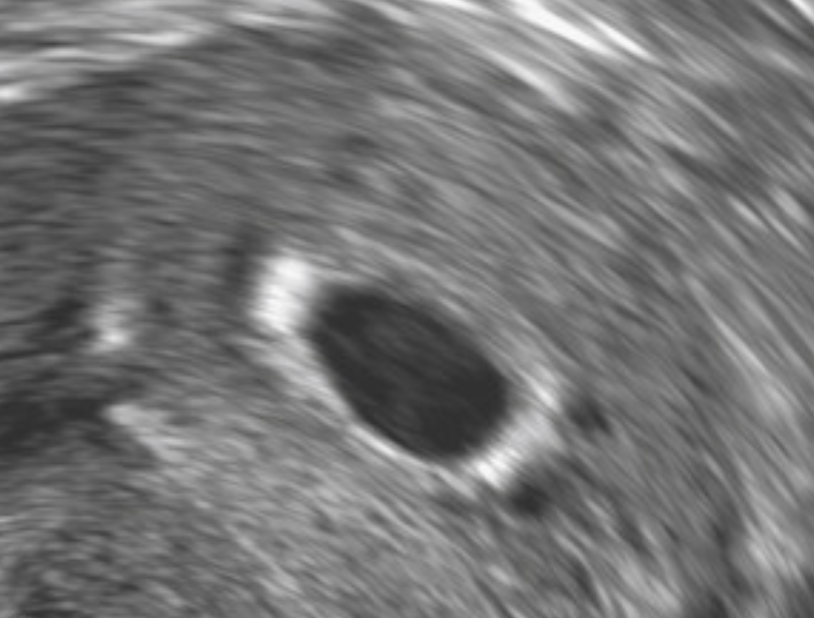
4-week gestation sac inside the uterus
Diagnosis isn't always straightforward, and it can take time. Not because your doctors don't know what they're doing, but because limitations of technology and testing mean that reliably diagnosing a miscarriage can only happen at specific stages of a baby's development.
A 7-week gestation sac (black circle) containing a yolk sac (smaller, brighter circle) and embryo
When a baby is 12 weeks along, and the heartbeat isn’t seen on ultrasound, there can be no doubt that a miscarriage has happened. But when a baby is much earlier - for example, only millimetres in size- the absence of a heartbeat could very well be a limitation of ultrasound accuracy. A heartbeat may be there, but it’s just not visible on the blurry screen in front of you.
Accurate cut-offs for diagnosing miscarriage are critical. If we make the diagnosis too early, we risk losing a much-wanted and viable pregnancy through miscarriage treatment. And delays in confirming what’s happening lead to more anxiety and stress.
Meaning of symptoms and ultrasound findings
So what are these clear criteria? Here's what the research tells us about meaning of symptoms, ultrasounds and some images to illustrate.
Embryo heartbeat measurement
A small amount of bleeding in early pregnancy does not increase the risk of miscarriage.
Heavy bleeding significantly increases the likelihood that a miscarriage will happen (30% vs 15% for no bleeding)
The presence of nausea and vomiting is a protective factor - miscarriage risk reduces to 9% if these are present
A gestation sac measurement of 25mm diameter or more and no visible embryo is diagnostic of miscarriage.
An embryo length of 7mm or more with no visible heartbeat is diagnostic of miscarriage.
Follow-up scan: 11 days or more after a gestation sac plus yolk sac was seen - if the next scan shows no live embryo - the diagnosis is miscarriage.
Follow-up scan: 14 days or more after a gestation sac, no yolk sac - if the next scan shows no live embryo, - the diagnosis is miscarriage.
A small embryo, no heart beat and a large gestation sac confirming miscarriage
What about smaller measurements than this on an ultrasound? Do they give any reassurance, or can they give you a guide to what’s happening?
If the gestation sac size is 16mm or greater, with no visible embryo, the miscarriage risk is 60%
If the gestation sac measures 20mm or more, with no visible embryo, the miscarriage risk is 70%
If the gestation sac measures 20mm or more, with no yolk sac, miscarriage is highly likely
Blood flow within tissue inside the uterus indicating an incomplete miscarriage
If embryo length is 5mm with no heartbeat, there is still a 45% likelihood that pregnancy will continue
If the embryo length is 6mm with no heartbeat, there is a 30% chance that the pregnancy will continue
As you can see, if the first ultrasound doesn’t give a clear answer to what’s happening, then a second scan 11-14 days later is needed to see if the pregnancy has progressed normally.
Often blood tests for the pregnancy hormone, hCG, are used to monitor progress until a gestation sac is seen. These blood tests are needed for diagnosing ectopic pregnancy but are less helpful for predicting miscarriage. If the hCG is falling, it’s an indication that miscarriage is likely.
After confirming a pregnancy sac inside the uterus, hCG levels are unlikely to give you the reassurance or the answers you need and a repeat ultrasound will provide the most accurate information.
When you’re closely watching a much-desired pregnancy, all this uncertainty can feel like torture - you just need to know what’s happening and where you stand so you can begin to process things. Often there is not a lot your treating team can do but give you accurate information and guide you through the process. Knowledge is power, and the above information is presented here not to confuse you but to help you understand what your treating team is thinking.
References
Australian Sonographers Association. Guideline for ultrasound diagnosis of early pregnancy loss. May 2022. Link (PDF). Main website.
Australian Society for Ultrasound in Medicine Guidelines. Link.