Pelvic Congestion Syndrome: a cause of chronic pelvic pain
Pain lasting longer than three months in medical terms is called ‘chronic’, and the recognised causes of pelvic pain haven’t changed for some time. Although Pelvic Congestion Syndrome has proven tricky to diagnose and treat, I recently saw two women with PCS in one week.
In the past, ultrasounds have sometimes identified enlarged pelvic veins. We’ve seen the same when we do a diagnostic laparoscopy, trying to get to the bottom of the cause. But the link to a specifically named and treatable condition has been lacking until recently.
Women with pelvic congestion syndrome (PCS) often spend months or years seeking help from doctors in various specialities, and many present firstly to their General Practitioner. Much PCS is undiagnosed because of our lack of familiarity with the condition.
PCS typically has the following features:
It usually occurs in women before menopause – but not always
Often after several pregnancies
It is associated with other vein-related disorders like varicose veins (80%) and vulval varicosities (24-40%), often with leg symptoms such as pain, swelling and heaviness.
Heavy lifting and prolonged standing are risk factors
Normal weight is more likely than not
Symptoms can include:
Chronic, dull pain on one or both sides
Pain increases during or after intercourse, leading to a throbbing ache afterwards
Pain can be worse throughout the day.
Worse pain in the days before and during the period
Symptoms may be reduced by lying down
What causes PCS?
As with varicose veins in the legs, there is likely a genetic predisposition – half of the varicose veins can be related to genetics. There may be an underlying weakness in the blood vessels, which makes them dilate more than usual. This can damage the valves inside the vein, which normally prevents back-flow. Hormonal factors can play a part, and oestrogen has been shown to weaken and swell veins – hence the link with pregnancy, a high state of oestrogen. There is also a higher blood volume in pregnancy, further stressing the leg and pelvis veins.
How is PCS diagnosed?
MRI with contrast showing the swollen ovarian veins on the right side of the image.
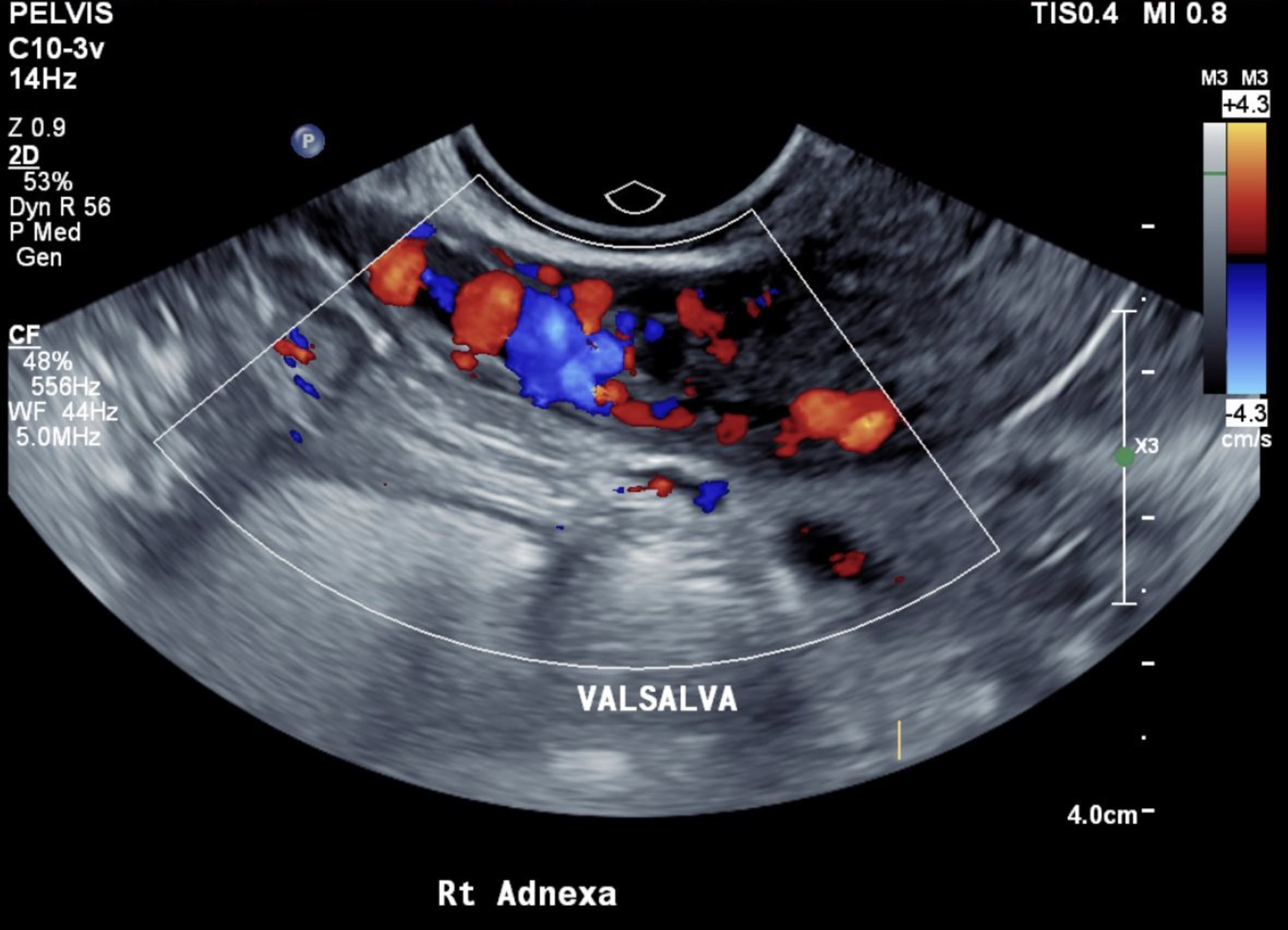
Ultrasound is the first line of screening and can show the enlarged, swollen veins, and they may swell further when you hold your breath and bear down – Valsalva manoeuvre. MRI can also be used, but the gold standard test is an investigation called venography. A radiology or vascular expert injects a dye into a vein below the area, and x-ray screening shows the dye filling the swollen vein complex. This is an invasive procedure, so it is generally only used as part of the treatment.
Many women with pelvic pain need diagnostic laparoscopy by a gynaecologist to rule out other common causes, such as endometriosis. However, the presenting symptoms and imaging may be clear in some cases. Laparoscopy may not show pelvic congestion due to positioning during surgery, and the gas used to create an operating space can make them collapse.
Treatment of PCS
Medical treatment has been tried, but the research studies are small. Depot provera injections plus psychotherapy had some success after nine months. Medical-grade compression shorts have been found to reduce pain and discomfort during sex in 80% of patients. But, not so comfortable in Queensland! Elastic stockings don’t help. There is a 20% recurrence rate after a hysterectomy, and one-third of women experience ongoing pain after this surgery.
The mainstay of treatment is embolisation of the veins to block off the blood flow and reduce swelling. This is usually done under sedation by a radiologist or vascular surgeon. Tiny beads/plugs or coils seal the veins, and success rates are between 47 and 100% - an average of 75% in the first three months after treatment.
There is still much to be studied – such as optimal treatment protocols and validated questionnaires to allow research comparisons.
Summary
Pelvic Congestion Syndrome is a common condition that occurs worldwide. Many cases are undiagnosed due to poor knowledge of the disease. Symptoms can be non-specific, and it can be hard to differentiate from other causes of pelvic pain. An awareness of the condition and ultrasound is the first step to diagnosing PCS and ruling out other conditions.
Ultrasound images showing pelvic venous congestion - ovarian veins more than 5mm diameter. Thank you to my two patients for permission to share their images.